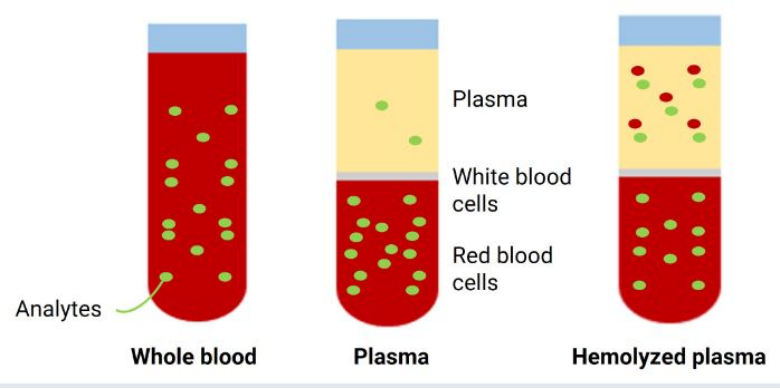
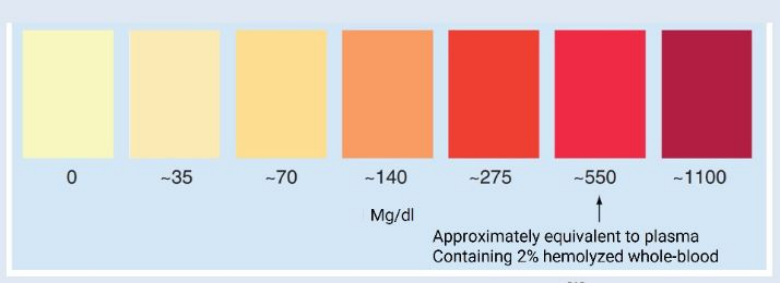
Hemolysis, the rupture of red blood cells (RBCs) resulting in the release of hemoglobin into plasma or serum, can significantly interfere with laboratory test results. It can skew the results of many diagnostic tests, including those measuring electrolytes, liver function, and enzyme levels. Proper sample collection and handling are critical to avoid hemolysis, ensuring the accuracy of laboratory analyses. In this article, we will explore the key steps in preparing samples for hemolysis analysis, focusing on the importance of collection techniques, handling, and storage.
Prepare Sample for Hemolysis Analysis
Here is how to prepare a sample for hemolysis analysis:
Selecting the Right Collection Tube
The first step in preventing hemolysis is choosing the appropriate collection tube. Blood samples are typically drawn into tubes that contain specific additives depending on the type of analysis required. For plasma or serum collection, it's essential to select the correct tube to minimize the risk of hemolysis. Tubes without additives are typically used for serum, while tubes with anticoagulants such as EDTA, heparin, or citrate are used for plasma. The tube should be handled with care to avoid any mechanical damage to the RBCs during collection. Excessive additives or incorrect tube types can contribute to hemolysis and impact lab results.
Proper Blood Collection Technique
The method used to collect blood plays a significant role in minimizing hemolysis. The size of the needle used for venipuncture is important; using a smaller needle may cause excessive pressure, leading to RBC rupture. To prevent this, a larger gauge needle should be used to facilitate smooth blood flow. Additionally, excessive suction during blood collection should be avoided. It is essential to handle the collection process gently, ensuring that the blood is not subjected to rapid or forceful movements, which could cause mechanical damage to the cells. Furthermore, applying a tourniquet too tightly or for too long can increase pressure in the veins and promote hemolysis, so it should only be used for a short duration.
Handling and Mixing of Samples
Once blood is collected into the tube, proper handling is crucial in preventing hemolysis. If anticoagulants are used in the collection tube, it is important to mix the sample gently by inverting the tube several times. Vigorous shaking should be avoided, as it can lead to the rupture of RBCs. Additionally, temperature is another factor to consider during sample handling. Extreme temperatures, either too hot or too cold, can cause RBCs to break down. Ideally, the sample should be kept at room temperature for the shortest possible time before being processed.
Ensuring Proper Centrifugation and Separation
After blood is collected and mixed properly, it is often necessary to separate the plasma or serum from the whole blood by centrifugation. To avoid hemolysis during this process, it is essential to ensure that the centrifuge is calibrated correctly and that the speed and time settings are appropriate. Over-speeding or prolonged centrifugation can cause RBCs to burst, leading to hemolysis. The sample should be centrifuged under the recommended conditions, and any excess force or inappropriate settings should be avoided. After centrifugation, the plasma or serum should be carefully transferred, avoiding any disruption of the blood cells.
Transport and Storage Considerations
Hemolysis can also occur during the transportation of blood samples to the laboratory. It is important to keep samples at the appropriate temperature to prevent changes that could lead to hemolysis. Samples should ideally be refrigerated if they cannot be processed immediately. Exposure to extreme temperatures, such as freezing or excessive heat, can accelerate the breakdown of RBCs. Additionally, samples should not be left in the collection tube for extended periods before processing, as RBCs may begin to break down naturally. Delays in processing can lead to spontaneous hemolysis.
Conclusion
Preventing hemolysis during blood sample collection, handling, and processing is essential for ensuring the accuracy of laboratory test results. From selecting the appropriate collection tubes to employing the correct techniques during blood collection and sample handling, each step plays a crucial role in minimizing the risk of hemolysis. Ultimately, understanding the hemolysis labs process and implementing best practices in sample preparation can lead to better diagnostic outcomes and improved patient care.